When Transporting A Patient With A Facial Injury for many healthcare providers, can evoke cringes and discomfort, if not outright dread. This unease often stems from the profound psychological and sociological significance we attribute to the human face. It serves as a conduit for recognizing friends and foes, expressing emotions, and conveying joy and pain. Consequently, facial injuries elicit strong emotional responses.
Beyond the emotional turmoil, facial trauma presents tangible, life-threatening risks. The brain, housing the vital airway origin, resides within the confines of the face. Moreover, forceful impacts to the face can disrupt the cervical spine, potentially leading to severe disability or even death. Injuries to these structures demand immediate recognition. Both visible and concealed injuries associated with facial trauma can exert grave consequences on a patient’s health and survival.
Anatomy
The musculoskeletal framework of the face is intricate, shaping its form. Notably, the central nervous system closely neighbors the visible face, with the posterior/internal face forming the anterior portion of the cranial vault, housing the brain. This proximity must be kept in mind when assessing facial injuries.
The face boasts a rich blood supply, featuring an extensive arterial and venous network. While most arterial supply originates from the facial and external temporal arteries, the ophthalmic artery, distinctively, emerges intracranially from the internal carotid artery before traversing the optic canal to nourish facial regions. This complex vasculature, unique to the face, often involves vessels crossing the midline to form anastomoses with contralateral vessels. As a result, injuries compromising facial vasculature, particularly the arteries, can lead to severe hemorrhage and, in rare cases, exsanguination. Controlling such hemorrhages proves challenging, given the absence of a single pressure point.
Facial innervation is another layer of complexity, mainly relying on cranial nerves. Cranial nerve VII, the facial nerve, governs most facial motor functions. Originating in the brainstem, it exits through the temporal bone and extends throughout the face. Injury to this nerve can result in debilitating facial paralysis. Sensation in the face is primarily mediated by the three branches of cranial nerve V, the trigeminal nerve. Any injury affecting these branches can lead to localized paresthesia.
Read More : How Much Tip For $150 Facial
Assessment & Management
Despite the emotional impact, the assessment and management of facial trauma follow a systematic approach akin to other injuries. Maintain focus, even in the face of severe injuries. Initiate the assessment by evaluating mental status; altered consciousness or unresponsiveness in the presence of facial trauma warrants heightened suspicion of traumatic brain injury.
Priority must always be given to maintaining a patent airway, as its compromise constitutes a medical emergency. Rapidly deploy an oral airway or oral endotracheal tube as necessary, avoiding nasopharyngeal interventions, which may pose risks, particularly with basilar skull fractures.
Direct airway trauma presents formidable challenges and may require invasive measures. Profuse hemorrhage, tissue disruption, or structural damage to the airway necessitates prompt and careful intervention. If airway compromise is impending, swift measures must secure and protect the airway. In dire cases where conventional methods such as oral airways, intubation, or adjunct airways are infeasible, immediate surgical airway establishment becomes imperative.
Following airway and breathing assessment, shift focus to circulation. Hemorrhage control takes precedence in facial trauma, although shock is rarely the initial presentation. Address facial hemorrhages through direct pressure and bulky dressings, ensuring frequent reassessment to detect any concealed bleeding.
A meticulous secondary survey of the face and head should follow the primary assessment. Vigilance for underlying injuries is paramount. The brain instinctively safeguards the face and head, considering them prime real estate due to housing four of the five senses. Facial injuries signal a breakdown in these protective mechanisms, and providers should remain vigilant, particularly when unexplained falls or syncopal events precede facial trauma.
While not detailed here, pain management remains a consideration for patients with facial injuries, as with any trauma patient.
Specific Facial Areas
Forehead & Orbits: The frontal bone forms the forehead and harbors frontal sinuses, vulnerable to fracture due to thinner walls. Orbital fractures, whether at the outer ring or deeper within the socket, manifest as pain, disfigurement, periorbital hematomas, or crepitus. Suspected or obvious ocular injuries demand immediate attention.
Maxilla & Nose: The maxilla, housing the upper gums, nose, and areas below the orbits, can suffer a range of injuries. Nasal fractures, common but weak, can disfigure the nose. Le Fort fractures, involving maxilla detachment from the skull, necessitate urgent intervention. Protecting the eye from further harm is paramount in cases of orbital injury.
Cheekbone: The zygomatic bone, forming the cheekbone, comprises a tunnel through which important structures for facial movement pass. Disruption to this canal may result in mandibular movement limitations.
Oral Cavity & Mandible: The mandible, housing the inferior gumline and teeth, stands as the sole mobile facial bone, responsible for jaw actions. Oral and mandibular trauma can introduce complications, with injuries ranging from superficial to requiring surgical repair. Mandibular fractures are relatively common among facial fractures and necessitate careful assessment for airway compromise.
Destination Criteria
Patients with significant facial trauma should be transported to appropriate facilities using suitable means. Air medical services are considerations for patients at risk of uncontrolled airway deterioration and facing prolonged transport times. These patients require transfer to trauma centers equipped with maxillofacial and plastic surgery services.
Read More : What Is Cryoskin Facial
Conclusion : When Transporting A Patient With A Facial Injury
While the anatomy and complexities of facial trauma are daunting, prehospital management remains straightforward. Maintaining vigilance for airway deterioration, intracranial pathology, and possible C-spine injury is paramount. Careful planning is crucial in addressing complications, ensuring that patients receive the high-quality care they deserve.


More Stories
Everything You Need to Know About Biomagnetic Cupping Therapy Sets
DIY Natural Remedies for Dandruff for Healthy Hair and Scalp
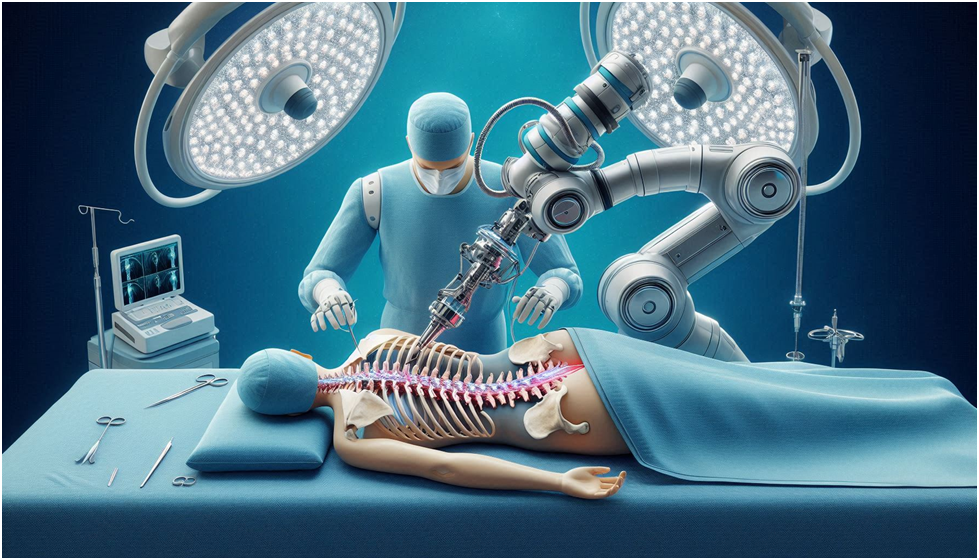
Revolutionizing Spinal Fusion: The Role of Modern Spine Implants